
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
The T1D Exchange Quality Improvement Collaborative (T1DX-QI) comprises 60+ endocrinology centers across the US, collectively caring for over 200,000 people living with type 1 and type 2 diabetes.
Our quality improvement coaches and data scientists work with healthcare providers at T1DX-QI member clinics to identify areas of unmet need, use data benchmarking, refine best practices, and implement evidence-based solutions that improve care and outcomes for people with diabetes.
This article delves into several recent research publications and presentations spearheaded by the T1DX-QI. These studies illustrate the collaborative’s efforts to improve glycemic outcomes, increase the use of diabetes technologies, and improve the overall care provided to people living with diabetes.
Learn more about our findings from each of these research studies:
- Implementing High-Risk Programs at Four Pediatric Endocrinology Clinics in the T1D Exchange QI Collaborative
- Improving glycemic outcomes for children and adolescents with type 1 diabetes: a T1DX-QI success story
- Insulin Delivery Devices in Management of T1D Among Pediatric Patients
- LGBTQ+ Supportive and Inclusive Care Practices: Survey Data from the T1D Exchange Quality Improvement Collaborative
- The Impact of War and Conflict on People Living with Diabetes: A Scoping Review
Implementing High-Risk Programs at Four Pediatric Endocrinology Clinics in the T1D Exchange QI Collaborative
The T1DX-QI piloted new high-risk programs at four pediatric diabetes clinics to help children with diabetes reach lower A1Cs.
The clinics created supportive programs for children with A1Cs of 9% or above. Rather than labeling these initiatives as “high-risk programs,” they emphasized the positive and supportive aspects of diabetes care.
The programs included a caring team of healthcare providers and educators who created personalized care plans for each child. These plans included education, regular check-ups, and person-centered care to meet individual needs.
Over 17 months, the average A1C levels among the children in these programs dropped by 2.5%. The study showed that supportive, personalized care can help improve outcomes for children with higher A1Cs.
Read this abstract and all abstracts from the 2024 T1DX-QI Learning Session.
Improving glycemic outcomes for children and adolescents with type 1 diabetes: a T1DX-QI success story
This study, presented at the International Society for Pediatric and Adolescent Diabetes’s 50th Annual Conference in October 2024, looked at how glycemic outcomes and diabetes device usage have changed at Rady Children’s Hospital-San Diego since they joined the T1DX-QI.
Participation in learning collaboratives can support benchmarking among clinics, executing improvement projects, and making system-level changes in the real world. Through their work with the T1DX-QI, Rady Children’s Hospital-San Diego aimed to increase the use of diabetes technologies like continuous glucose monitors (CGMs) and insulin pumps, encourage more frequent clinic visits, and provide better support for at-risk children.
Over four years, we found the following improvements:
- CGM usage rose from about 60% to over 90%.
- Insulin pump usage increased from about 29% to 50%.
- Average A1C dropped from 8.7% to 8.1%.
- The number of children with an A1C below 7% increased by 11.3%.
In summary, sharing best practices and using improvement science through the T1DX-QI may have led to increased use of essential diabetes tech and improved glucose management in young people with type 1 diabetes.
Read the full abstract on page 191 of the 2024 ISPAD Abstract Book.
Insulin Delivery Devices in Management of T1D Among Pediatric Patients
Jackson Medical Health System/University of Miami, an endocrinology center in the T1DX-QI, conducted a study to compare different insulin delivery methods for children with type 1 diabetes and their impact on A1Cs.
The methods studied included multiple daily injections, smart pens, insulin pumps without automated insulin delivery (non-hybrid pumps), and automated insulin delivery systems (hybrid insulin pumps.)
Overall usage of each insulin delivery method:
- Hybrid pumps: 44%
- Non-hybrid pumps: 8%
- Smart pens: 24%
- Multiple daily injections: 25%
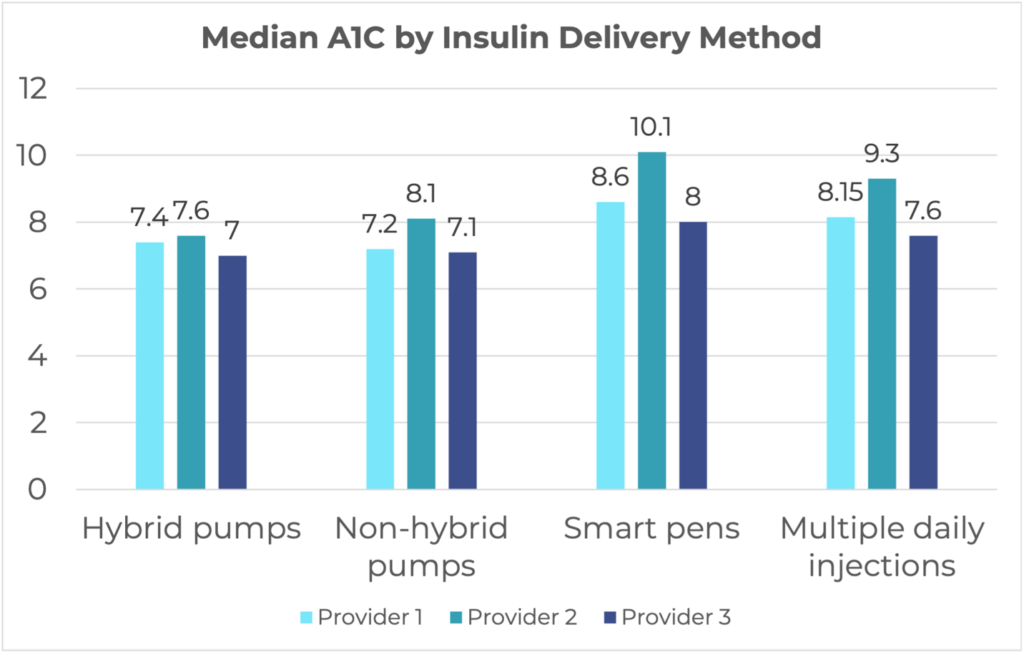
The study found that hybrid pump users had the lowest median A1C, and non-hybrid pump users had the second lowest. The highest median A1C was among smartpen users.
The success of insulin delivery devices varied among the three healthcare providers involved in this study and their patients. The study notes that Provider 2’s patients mostly had public insurance. Other factors, such as a person’s device preference and correct usage, might also influence these results.
Read this abstract and all abstracts from the 2024 T1DX-QI Learning Session.
LGBTQ+ Supportive and Inclusive Care Practices: Survey Data from the T1D Exchange Quality Improvement Collaborative
Living with type 1 diabetes is tough, and LGBTQ+ (lesbian, gay, bisexual, transgender, queer, or other gender-expansive identities) individuals can face additional barriers.
Recognizing the need for personalized care for these individuals, the Health Resources and Services Administration requires medical centers to document their patients’ sexual orientation and gender identity (SOGI). We surveyed 50 diabetes care centers in the T1DX-QI to understand the current practices around documenting this information.
Here’s what we learned:
- 64% of pediatric centers had strategies in place for SOGI documentation.
- 50% of adult centers had implemented strategies for SOGI documentation.
- Some adult centers could not confirm whether they recorded this information.
Overall, while most centers recorded gender identity and pronouns, fewer documented sexual orientation. More work is needed to standardize SOGI documentation practices and to understand its impact on LGBTQ+ people with diabetes.
Read the full article in DiabetesSpectrum.
The Impact of War and Conflict on People Living with Diabetes: A Scoping Review
War and conflict can severely affect people living with diabetes. The T1DX-QI reviewed research from 1950 to 2023 to understand how war impacts diabetes management and health.
The findings highlighted three main issues:
- People in war zones often have higher glucose levels.
- The stress of living in conflict areas makes it harder for people to manage their diabetes and reduces their quality of life.
- Access to healthcare, including necessary medications and services, is often disrupted during war.
Overall, the findings emphasize the profound impact of war and conflict on people living with diabetes. This review shows a need for more research to identify the factors that worsen these challenges and find ways to help people with diabetes in conflict settings.







