
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
Our mission at the T1D Exchange is to improve the lives of people with type 1 diabetes (T1D). A large part of how we accomplish this mission is through research.
At the T1D Exchange, our Outcomes Research team collaborates with leaders in the T1D space and other experts at T1D Exchange to design studies to understand the preferences, experiences, and quality of life of people living with T1D in our Registry and Online Community.
If you are a part of the Registry, you’ve likely seen study opportunities on your dashboard. You may have even participated in some of these studies! And you may have wondered what happens after you participate?
Here, we’ll highlight the results of one of our recent studies on emergency glucagon: Emerging Adult and Caregiver Psychosocial Experiences with Severe Hypoglycemic Events and the Perceived Impact of Nasal Glucagon: A Cross-Sectional Study, which was recently published in Diabetes Therapy.
What is severe hypoglycemia?
Before we get into what we did in this study, it may help to understand the why behind the science.
If you have lived with T1D or been a caretaker to someone with T1D, you know that severe low blood glucose events (“severe lows”) are rather inevitable when using insulin and trying to achieve target blood glucose goals.
A severe low —or, in medical terms, a severe hypoglycemic event — is a low blood glucose that is so low it impairs a person’s functioning to the point that they need someone else to help them recover. Impaired functioning may look different in different people but often includes the person with T1D becoming confused or losing the ability to speak coherently, passing out (or losing consciousness), and — eventually, if it’s low enough — suffering from a seizure. Severe lows are life-threatening medical emergencies.
In addition to being a physical medical emergency, severe lows and the potential for severe lows are also emotionally charged events. People with T1D often report distress and anxiety about severe lows, and fear of hypoglycemia is a common experience for many.
Glucagon: a life-saving hormone in T1D
Glucagon is a hormone that helps to keep blood glucose from going too low by telling your liver to break down glycogen into glucose and signaling your body in other ways to break down glucose. While glucagon is naturally produced in the body, in people with T1D, this life-saving mechanism doesn’t function properly.
That’s where “emergency glucagon” fills this gap for people with T1D. Glucagon can be an effective treatment for severe lows. However, despite advancements in emergency glucagon devices, few people use it for many reasons.
Unfortunately, the original “emergency glucagon kit” gave glucagon a difficult reputation. Many people find it difficult to use, requiring multiple steps of mixing liquid with a messy powder and then giving a muscular injection during an already extremely stressful emergency.
Fortunately, there are single-step glucagon devices that are intended to be easier to administer during a severe low.
Most of the research, however, with newer formulations, focuses on the effectiveness of the glucagon device or using the device in simulated events rather than the perceptions and real-world experiences of people with T1D.
So, with our amazing collaborators at Eli Lilly, we designed a study to explore these real-world perceptions and experiences in people who were familiar with both injectable glucagon that requires reconstitution and nasal glucagon — a newer formulation of glucagon that comes in a powder and is passively absorbed in the nasal passages.
Perceptions and Experiences with Severe Lows and Glucagon in Young Adults and Caregivers
Study Overview
Young adults experience many changes in their daily lives that impact their T1D management — they move away from their parent home for the first time and are primarily responsible for their T1D management compared to younger teens and children.
For young adults, a potential severe low may be especially distressing or challenging in these new environments where they are responsible for enlisting others to help in the event of a severe low. While caregivers (such as parents) are also distressed by severe lows, there could be important differences between young adult experiences and caregiver experiences.
We recruited and enrolled three groups of participants (364 young adults, 138 caregivers of a young adult, and 315 caregivers of a child/teen) in our study to explore real-world perceptions and experiences in answering three questions:
- How do young adults and caregivers think about distress from potential severe lows, and how do they think about the process of enlisting other people to help in the event of a severe low?
- Since adding nasal glucagon to their available options to treat a severe low, do young adults and caregivers perceive any changes or impact of how distressed they feel about a potential severe low or how they feel about the process of enlisting others to help?
- How prepared and protected do young adults and caregivers feel about severe lows when thinking about nasal glucagon compared to traditional injectable glucagon that needs to be reconstituted from a powder to a liquid?
Summary of Results
In the graphic below, you’ll see an overview of our findings.
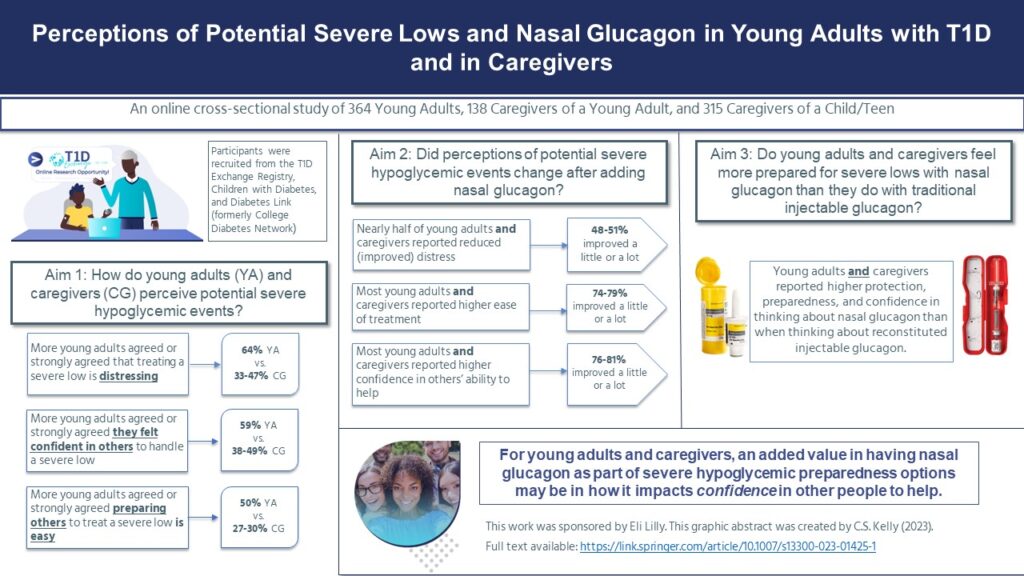 There were some differences in how young adults perceived severe lows compared to caregivers. More young adults agreed or strongly agreed that severe lows were distressing. However, young adults also expressed more confidence and greater ease in preparing others to help them with a severe low.
There were some differences in how young adults perceived severe lows compared to caregivers. More young adults agreed or strongly agreed that severe lows were distressing. However, young adults also expressed more confidence and greater ease in preparing others to help them with a severe low.
There were also some similarities between young adults and caregivers’ perceptions of severe lows. Most young adults and caregivers reported that since adding nasal glucagon to their treatment options for a severe low, their perceptions of how easy it is to treat a low and their confidence in other people to help improved.
When we compared perceptions of nasal glucagon to their perceptions of traditional glucagon, young adults and caregivers reported higher preparedness, protection, and confidence in nasal glucagon.
Conclusions and Implications: The ‘So What?’ Summary
We knew going into this study that nasal glucagon is an effective treatment for severe lows. How do people think about nasal glucagon in the real world?
We concluded that — in general — nasal glucagon may provide some additional benefits to people with T1D beyond the physical benefit of resolving a medical emergency. Specifically, that nasal glucagon may help to increase confidence in others’ ability to help.
While we need more research to further understand the implications of this finding, it provides some preliminary evidence that perhaps newer formulations of glucagon such as nasal glucagon could help bolster the number of people young adults and caregivers perceive could be ‘people to count on’ during an emergency.
The increased confidence and perceived greater ability of having others around who could help in turn may also decrease some of the distress people with T1D have about potential severe lows. Decreasing some of the distress experienced about severe lows would be a — perhaps small but meaningful — way to improve the lives of people living with and affected by T1D!
Caitlin Kelly
Related Stories
1 Comment
Perceptions About Nasal Glucagon in Young Adults and Caregivers Cancel reply
You must be logged in to post a comment.








The real world — that one that all of us actually experience, behave, & live in — is markedly different from the ivory tower Panglossian world researchers often float around in. Simplicity, simplicity, simplicity are the 3 principles for anyone else helping out. So what? The easier and quicker the administration of aid and assistance become, the better the outcomes. Good research. Thanks.