
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
From technology to mental health, this year’s research from T1D Exchange highlighted where progress is happening—and where gaps remain—in diabetes care.
Below, we’ve rounded up our most viewed research published in 2025!
Diabetes Technology
Early continuous glucose monitor use can improve long-term outcomes in youth.
This study from the T1D Exchange Quality Improvement Collaborative (T1DX-QI) found that starting continuous glucose monitor (CGM) soon after a type 1 diabetes (T1D) diagnosis—ideally within the first six months—may help children and teens have better long-term health outcomes.
For this study, healthcare providers in the T1DX-QI clinic network tracked over 4,000 children and adolescents for three years following their diagnosis of T1D. Most (93%) began using a CGM at some point in those three years, but the timing varied—some started within the first few months, while others waited a year or more.
We found that the children who started using a CGM within the first six months after diagnosis had lower A1Cs three years later, compared to those who started later or never used a CGM.
Read the full article in Diabetes Care.
Starting automated insulin delivery early can improve outcomes for children with T1D.

These study results, presented at the 2025 Advanced Technologies & Treatments for Diabetes (ATTD) conference, explored whether initiating automated insulin delivery (AID) soon after a T1D diagnosis leads to better outcomes for children and teens. Using electronic health record data from more than 44,000 youth in the T1DX-QI, researchers compared outcomes two years after diagnosis based on when they started using an AID system.
Children who began AID within six months had lower A1C levels and significantly fewer episodes of severe hypoglycemia and diabetic ketoacidosis (DKA) than those who started later or did not use AID. Early AID use was associated with better overall diabetes management.
Read more at OP012 / #789 in the ATTD 2025 DTT Journal.
Young adults with T1D are less likely to use technology in adult care.
This study, also presented at the 2025 ATTD conference, compared emerging adults (aged 18-23 years) with T1D receiving care in pediatric versus adult institutions.
Using data from the T1DX-QI, the researchers analyzed 8,538 young adults from pediatric centers and 839 from adult centers.
They found that the individuals in adult institutions were generally more likely to have an A1C of 9% or higher and were less likely to use diabetes technologies such as CGMs and insulin pumps.
Read more at EPD063 / #187 in the ATTD 2025 DTT Journal.
Adjunctive Therapies
Combining CGM and GLP-1 therapy leads to greater A1C reductions.
This study, presented at the American Diabetes Association’s (ADA) 85th Scientific Sessions, looked at real-world data to see whether pairing CGM with GLP-1 medications leads to better glucose outcomes for adults with type 2 diabetes. On their own, both tools helped—GLP-1 therapy lowered A1C by 0.4%, and CGM use lowered it by 0.5%.
However, the largest improvement occurred when people used both at the same time, with A1C levels dropping by 0.8%. Together, the results suggest that combining CGM and GLP-1 therapy can deliver greater benefits than either approach alone.
Inhaled insulin users report high satisfaction, but face cost barriers.
At the 2025 Association of Diabetes Care & Education Specialists (ADCES) conference, the T1D Exchange Research team presented new insights into what it’s actually like to use inhaled insulin.
A significant majority of current inhaled insulin users reported being highly satisfied, intended to continue using it, and said they would strongly encourage family and friends to consider using inhaled insulin. Most people who have used inhaled insulin, including those who do not currently use it, have seen improvements in their quality of life.
However, high costs and insurance barriers, such as prior authorizations and insurance coverage denials, can make access to inhaled insulin difficult.
Learn more about our inhaled insulin research.
Comorbidities
20% of T1D Exchange Registry participants have 2+ musculoskeletal conditions.
These insights from the T1D Exchange Registry, presented at the 2025 ADA Scientific Sessions, showed that people with T1D may be more likely to experience certain joint and muscle-related (musculoskeletal) conditions. We analyzed data from our online registry of people with T1D to determine the prevalence of these issues.
We found that 20% of people reported having two or more musculoskeletal conditions at some point in their lifetime. These conditions were more common in women, older adults, and those who had lived with diabetes for a long time. We also found that people with a higher body mass index were more likely to have multiple musculoskeletal conditions.
Chronic kidney disease in adults with T1D is linked to slightly higher DKA risk.
Presented at ATTD, this study analyzed electronic health record data from nearly 50,000 adults with T1D to examine the impact of chronic kidney disease (CKD) on DKA and severe hypoglycemia. About 3% of participants had CKD and were older with longer diabetes duration.
Once differences in age, demographics, and treatment methods were taken into account, severe hypoglycemia occurred at similar rates in people with and without CKD. In contrast, adults with both T1D and CKD showed a small but meaningful increase in DKA risk.
Read the full abstract at EPD087 / #922 in the ATTD 2025 DTT Journal.
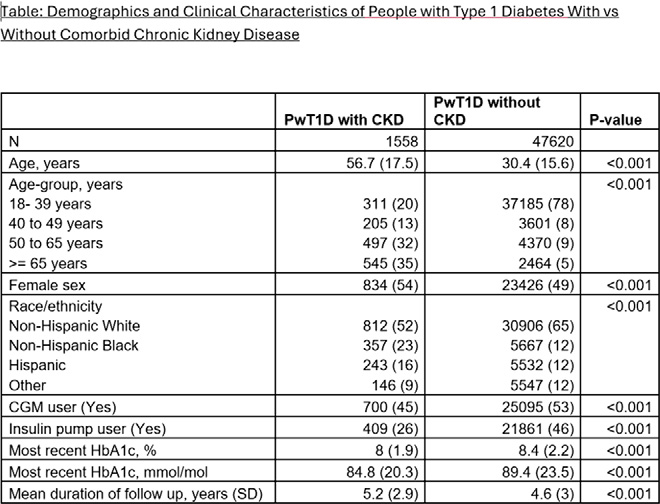
Adults with T1D and CKD use diabetes technology less often.
Similar to the above ATTD presentation, we used electronic health record data from the T1DX-QI to compare demographic characteristics and health outcomes between people with T1D who have CKD and those who do not.
We found that adults with CKD included nearly twice as many non-Hispanic Black individuals (23% vs. 12%), were less likely to use insulin pumps (26% vs. 46%) or CGMs (45% vs. 53%), and had slightly lower average A1C levels (8.0% vs. 8.4% in people without CKD).
Read the full abstract at EPV441 / #990 in the ATTD 2025 DTT Journal.
Mental Health
Financial stress is common in T1D and linked to worse outcomes.
This project, presented at ADA, examined the financial impact of managing T1D and how financial strain may affect health.
Our researchers surveyed over 1,200 adults with T1D in our registry and found that 54% experienced financial stress due to the ongoing costs of medications and care.
Participants with higher financial strain had higher A1C levels, and high stress was more prevalent among lower-income individuals, those with less education, women, and non-White participants.
We also found that higher financial stress was associated with increased mental health challenges, like anxiety and depression, as well as with serious health events like DKA and severe hypoglycemia.
Diabetes distress screening remains limited in routine care.
National guidelines recommend routine screening for diabetes distress because it can affect both physical health and quality of life. To understand how often this happens in practice, we surveyed 57 endocrinology clinics in the T1DX-QI network and presented the results at ADA’s Scientific Sessions.
Only 35% of clinics reported screening people with T1D or their caregivers for diabetes distress, with pediatric clinics more likely to screen than adult clinics. Just 16% of clinics screened more than half of their T1D population each year.







