
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
The T1D Exchange Quality Improvement Collaborative (T1DX-QI) Learning Sessions “Five years of T1DX QI Collaborative and Reimagining the Future of Diabetes Care,” took place virtually, in partnership with Boston Medical Center, on November 8th and 9th. The Learning Sessions explored type 1 diabetes (T1D) quality improvement (QI) initiatives underway across the U.S., in addition to novel therapies, strategic approaches, and interventions to improve T1D care.
Formative groundwork for T1DX-QI was laid between 2014 and 2016, including a pilot phase spearheaded by experts from 10 diabetes centers. With formal establishment in 2016, T1DX-QI has seen tremendous growth; at present, there are 43 endocrine clinics involved in testing and implementing scalable, real-world solutions for diabetes care. T1DX-QI is comprised of thought leaders, clinicians, people living with T1D, and other key stakeholders; clinical partners serve a base of approximately 55,000 people living with T1D.
“We’ve been on a journey, and it’s been shared by many. This learning session really reflects on the last five years, what we’ve achieved, and what the future holds for us as a network,” said, Osagie Ebekozien, MD, MPH, CPHQ, Chief Medical Officer and Executive Vice President at T1D Exchange in his opening remarks. Ebekozien went on to express his gratitude for the Helmsley Charitable Trust, diabetes leaders, and innovators who have helped to sustain T1DX-QI’s important work.
T1DX-QI objectives include:
- Collecting data to drive improvements and help to shape T1D decision making
- Collaboratively designing and testing ideas to improve outcomes
- Calculating and understanding measures that make quality improvements
- Developing insights and change packages (how-to guides) to share broadly
- Utilizing the QI portal for benchmarking and improvements in population health
There have been an astounding 61 QI projects completed in 2021, including the following special projects: COVID-19 Surveillance Study, New Diagnosis and DKA Trends Study, Telemedicine Study, Smartpen Provider Study, Clinic Practices Survey, Health Equity Advancement Lab (HEAL), a type 2 diabetes Pilot, and a Fear of Hypoglycemia Study.
While Dr. Ebekozien reflected on the T1DX-QI’s goals, accomplishments, and gains, he expressed excitement about future objectives, too. “We should be proud to celebrate this as a network. We’re excited for 2022 and beyond, and to continue to partner with Helmsley and other funders to really expand the work that we’re doing: transforming QI culture, A1c improvements and beyond, real-world data, psychosocial care, and health equity.”
“We’re really proud to have shared this session with T1DX-QI members, to learn with and from each other, in an environment that encourages open sharing and reciprocity. We’re inspired as we explore ways to improve care together over the next five years, and continue to improve diabetes health outcomes, equitably, through this population health program,” said Nicole Rioles, Director of Clinical Partnerships and Population Health at T1D Exchange.

During the 2021 Learning Sessions, 21 abstracts were presented and published in the Journal of Diabetes. They included work on infrastructural support of the T1DX-QI, developing population health initiatives, improving T1D psychosocial support, and closing inequities in access to diabetes technology.
The collaborative not only provides peer-to-peer knowledge sharing and resources to identify and address gaps in care, but T1DX-QI studies continue to yield critical information to help people living with diabetes to live healthier, satisfying, and longer lives.
Highlights from two Learning Session presentations
Nourishing our Community: Use of Teaching Kitchen, Rooftop Farm, and Preventive Food Pantry in Diabetes Care, presented by Ivania Rizzo, MD, Endocrinologist, Assistant Professor, Director of Obesity Medicine at Boston Medical Center, and Olivia Weinstein, MS, RD, LDN, Culinary Nutrition Director of the Teaching Kitchen at Boston Medical Center.
Nourishing our Community is a cutting-edge program established in 2001, with a focus on addressing social determinants of health — specifically food access — utilizing a three-pronged program: A Teaching Kitchen, Rooftop Farm, and Preventive Food Pantry for a diverse, underserved, inner-city community. This is the first hospital-based food pantry in the U.S. The program fits into BMC’s mission to not only care for patients regardless of their ability to pay, but also to provide services to support the community’s overall health.
Dr. Rizzo highlighted that “low income households disproportionately struggle to meet basic needs,” such as food and payments for homes. There is also a greater struggle with higher rates of depression, which may lead to a lack of hope; Rizzo explained, “although BMC has many challenges, we also have many opportunities to assist these patients,” and that’s just what they achieved.
Their success starts by screening people with T1D for food insecurities, followed by an electronic medical record referral. BMC serves 80,000 people in this program yearly, with children accounting for 40% of that population. The rooftop farm was built in 2018, and harvested produce is served in the cafeteria, on inpatient food trays, and used in the food pantry. The teaching kitchen is located at BMC, but they have offered virtual programs for patients, staff, and the surrounding community since COVID-19.
With BMC’s “Eat to Treat” program, food conversations start at in-clinic visits with providers guiding individuals with T1D through the phases of assessment, referral, and treatment with medically-optimized foods. In 2021, they also piloted virtual, shared medical visits as part of the care model. BMC intends to collaborate with other institutions to disseminate their learnings for wider adoption and improved outcomes for all.
Innovations in Pediatrics Care, presented by Daniel DeSalvo, MD, Assistant Professor at Baylor College of Medicine and a Pediatric Endocrinologist at Texas Children’s Hospital and Linda DiMeglio, MD, MPH, Professor of Pediatrics at Indiana University School of Medicine and Division Chief of Pediatric Endocrinology and Diabetology.
Dr. DeSalvo highlighted progress made in the pediatric space over the last 5 years, in conjunction with the T1DX-QI, which included: pediatric studies, QI methodologies, improved outcomes, and shared knowledge. He expanded on a handful of issues tied to rising A1c values (regardless of improvements that we’ve seen in terms of technology and the delivery of care), they included:
- gaps in care delivery
- unmet psychosocial needs
- diabetes self-management burdens
- suboptimal healthcare designs, and
- health disparities
DeSalvo pointed out that care needs to be altered, “from acute and reactive — to proactive, planned, and population-based.” He suggests that “informed, activated patients and a prepared proactive practice team can optimize and improve outcomes over time,” adding that systematic QI methods can lead the charge to measurable improvements.
“QI collaboratives really enable an organized multi-faceted approach, which includes teams from multiple healthcare systems like ours, that can unite together to develop, apply, and disseminate initiatives.” And he reminds that sharing best practices and involving patients and families are a vital part of accelerating improvements in diabetes care.
Dr. DiMeglio spoke on Reimagining the Future of Diabetes Care, peering into the next 5 years, while celebrating advancements in diabetes care, such as the 100th anniversary of the discovery of insulin. “Despite the advancements we’ve made, we’ve yet to meet the strides we need to care for persons with diabetes,” QI work must continue, reminded DiMeglio, who addressed 4 domains for future advances in T1D care including: Care, education, policy/access, and a T1D cure.
Here is a glance at a few abstracts that were presented at the T1D Exchange Learning Sessions. A full list of published abstracts can be found in the Journal of Diabetes.
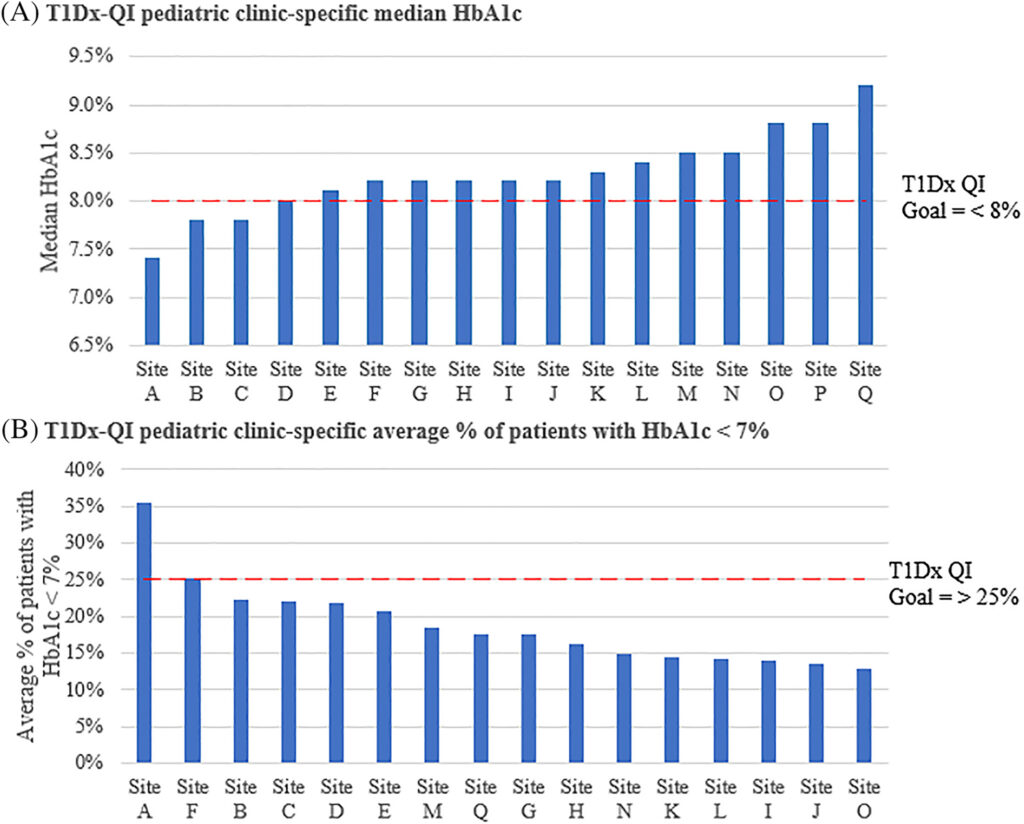
- Benchmarking HbA1c targets across T1D exchange quality improvement pediatric clinics Data sharing framework allows for benchmarking (performance comparison) amongst T1DX-QI clinics. This T1D Exchange study shows that through shared knowledge, effective QI strategies, and tools provided to partner clinics can improve outcomes with A1c averages. Two collaborative goals included: decreasing median A1c to <8% and increasing the percent of patients with A1c values of <7%.
- Improving access to continuous glucose monitors (CGMs) for high-risk patients
This University of Alabama study was focused on increasing the amount of prescribed CGMs for high-risk patients. With Alabama’s focused QI efforts, CGM use increased in this cohort from 35% to a sustained 85%. - Medicaid coverage of CGM in Texas: A quality improvement success story in advocacy
This Texas Children’s Hospital study had a QI focus on improving CGM access for children on Texas Medicaid. With the QI advocacy of diabetes care providers, patients, and families, Texas Children’s CGM use for this population rose above 60% from a baseline of 8%.







