
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
T1D Exchange sat down with Daniel DeSalvo, MD, a pediatric endocrinologist at Texas Children’s Pediatric Diabetes Center, for a Q&A on glucagon use with type 1 diabetes (T1D).
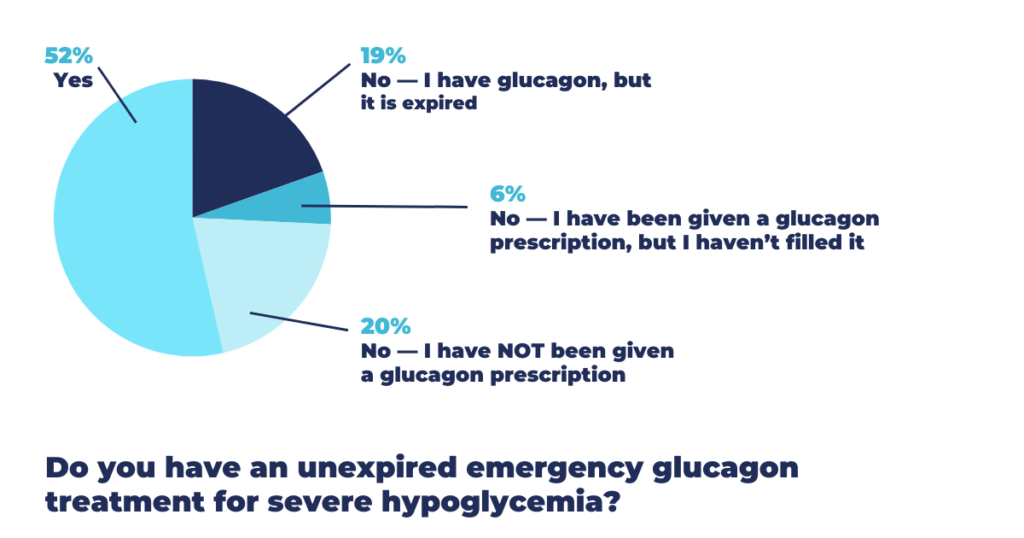
We sought Dr. DeSalvo’s expert opinions to share with you, having noted responses to a recent T1D Exchange Question of the Day: “Do you have an unexpired emergency glucagon treatment for severe hypoglycemia?”
With about 250 respondents, only 52% reported having an unexpired emergency glucagon treatment for severe hypoglycemia, 20% reported never receiving a glucagon prescription, 19% reported having an expired prescription, and 6% reported having an unfilled glucagon prescription.
“These responses really highlight the need to have prescriptions for glucagon given, expiration dates checked, having it readily accessible, and teaching others how to give it in the event of an emergency,” said Dr. DeSalvo.
What is emergency glucagon, and how does it work?
Glucagon is a medication that can be given to someone who is having a severe hypoglycemic event. That’s when someone’s blood sugar is so low that they pass out (lose consciousness) — or they cannot take things by mouth.
Glucagon can be prescribed in two forms: as an injection or as a medication that’s inhaled through the nose. Both work by helping to mobilize glycogen (glucose) stores in the liver to raise a person’s blood glucose level.
Why is it essential for people taking insulin to have unexpired glucagon on hand?
If someone has an unexpected severe low, giving glucagon can bring their blood glucose up, essentially rescuing someone from a severe hypoglycemic event.
What’s your elevator pitch to encourage people to fill their glucagon prescriptions? (For example, someone may think I’ve never needed glucagon, it’s expensive, it expires, etc.)
My elevator pitch is quite simple: Glucagon is a medicine that can save your life. Even if you’ve gone many years without experiencing a severe hypoglycemic event, you still need to have glucagon available — no matter what. It can happen when you least expect it.
What’s the rule of thumb for giving glucagon?
A good rule of thumb is that if you have low blood glucose or a hypoglycemic event, where you can’t take things by mouth (rapid-acting carbs), then it’s a good time to take glucagon.
And, if someone with diabetes is found down, has lost consciousness, or has had a seizure, those would also be indications to give glucagon.
If glucagon is administered, should 911 be called?
It’s a good idea to call 911 if you’ve given glucagon for a loss of consciousness or a seizure. This way, emergency care can be given to the person with diabetes.
While it’s most likely that their blood glucose will come up after glucagon is given, it’s still smart to call for emergency help. We give this advice at Texas Children’s Diabetes Care Center to children, youth, and families who live with type 1 diabetes.
When you prescribe glucagon, how do you decide between a nasal or injectable formulation? (Baqsimi®, Gvoke HypoPen®, Gvoke Kit®, Zegalogue®)
In my practice for students at school, where there’s a nurse, I want to ensure they have glucagon on hand, whether that’s Baqsimi, Gvoke, or Zegalogue. While it may be easier to give Baqsimi because it’s nasal glucagon, Gvoke and Zegalogue are liquid stable forms of glucagon — so they’re also very easy to inject.
Traditional glucagon kits had many steps, and it was a lot more challenging to give. Baqsimi, Gvoke, or Zegalogue are preferred and prescribed depending on insurance coverage.
For individuals who are going off to college or living with a new roommate, or for someone who is less used to injecting medications, Baqsimi is a great option: It’s easy to give, passively inhaled, and pretty foolproof. You just put a puff into the nose, and as it’s absorbed, it will help increase glucose levels.
Have the newer, easier-to-use formulations increased the use of glucagon in emergencies?
The short answer is yes. Off-the-shelf, ready-to-give forms of glucagon really help the person giving it in an emergency. That’s because with newer forms of glucagon, you don’t have to reconstitute the vial with a diluent, so it’s much easier to give.
When a person with diabetes has lost consciousness or maybe had a seizure, it can be a really frightening experience for the person helping them. Giving the old form of glucagon with its many steps — when a person was already emotionally rattled — was challenging. Now that we have these new, easy-to-give forms of glucagon, they’ve simplified the process of giving it in an emergency.
Let’s talk about microdosing glucagon. Can you explain what this means?
Suppose someone has an illness (i.e., a gastrointestinal issue with nausea and vomiting) and has a mild hypoglycemic event but can’t hold things down. In that case, a mini-dose of glucagon can be enough to get glucose up without causing rebound hyperglycemia (or nausea/vomiting that can happen with a full dose of glucagon).
The new liquid-stable forms of glucagon are made to deliver as a full dose in an emergency. Hopefully, the makers of Gvoke and Zegalogue will have options for mini-dose glucagon in the future.
Again, microdosing glucagon is not recommended in a severe hypoglycemic emergency. When a person has severe hypoglycemia (loss of consciousness, seizure, or incoherence and can’t take things by mouth), they’ll need a full dose of glucagon according to what has been prescribed. Dosing may vary depending on a person’s age and size.
How do I request a glucagon prescription?
If you’re receiving care from an endocrinologist, they know about glucagon and can easily prescribe it. If you’re seeing a health care provider who is a family practice or internal medicine doctor, they should also know about it.
If your provider isn’t aware of glucagon for some reason, it’s important that you are empowered with knowledge about glucagon so you can request a prescription with refills.
I always prescribe a two-pack kit of glucagon. That way, you can have one at home, and another at school, work, or with a different caregiver. Keep your provider in the loop. As a pediatric endocrinologist, I want to know if one of my patients has needed emergency glucagon because changes in management may be required.
Can you address preparedness for a severe low? The where (it’s kept), when (to give), and how (to administer)
You’ll want to make sure glucagon is kept in a place that’s easy to find and readily accessible. That way, if a severe hypoglycemic event occurs, it can be given immediately.
Instructions need to be clear: If there’s a seizure or loss of consciousness, give glucagon. By teaching others how to administer glucagon, a loved one, teacher, or friend will be prepared in case of an emergency.
Dr. DeSalvo: The Bottom Line
I want to give a special thanks to T1D Exchange for highlighting glucagon, a truly life-saving medication for people with diabetes who are taking insulin.
While technology such as continuous glucose monitors (CGMs) and automated insulin delivery (AID) systems are helping to reduce the occurrence of severe hypoglycemia, they aren’t perfect solutions. Severe low glucose can still occur, and you may need glucagon as a life-saving measure. That’s why it’s so important to have unexpired glucagon on hand.







