Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
Autoimmunity: The Breakdown
In honor of National Autoimmune Awareness Month, T1D Exchange would like to raise awareness and understanding of other autoimmune diseases affecting our community.
Did you know having one autoimmune condition places you at higher risk of developing another? Research suggests about one in every five people who live with type 1 diabetes (T1D) go on to develop another autoimmune condition in their lifetime.
While experts continue to learn more about autoimmune disease, for now, they are not entirely sure why it happens. If you live with T1D and notice telltale signs of another autoimmune disease, speak up about your concerns. Self-advocacy can lead to early recognition and improved outcomes. Let’s take a closer look.
What is autoimmune disease?
The immune system is built to protect the body from disease and infection, but sometimes it becomes confused, attacking its healthy parts instead. When this happens, a person may notice symptoms of autoimmune disease.
Some of these attacks can be more harmful than others, targeting any part of the body. T1D is an organ-specific autoimmune disease, meaning the body attacks a single organ — the insulin-producing pancreas.
Other autoimmune conditions are non-organ specific, meaning autoimmune activity can be spread throughout the body, resulting in various symptoms. Exactly what triggers autoimmune disease is unknown, and each person’s experience with autoimmune conditions can be different.
What we do know is that women are up to four times more likely to develop autoimmune disease than men, and a combination of genetics, environment, and lifestyle likely play a role. More research is needed.
Autoimmune conditions
Anyone can develop one of the more than 100 autoimmune conditions that exist, but again, some people are at higher risk.
Autoimmune disease also tends to run in families. This does not mean everyone in your family will have the same diagnosis, but it does mean that if someone has an autoimmune condition, others may have one as well.
Put another way, if you live with T1D, family members may have lupus, rheumatoid arthritis, or inflammatory bowel disease, for example — not just T1D.
While there is no cure for life-long autoimmune diseases, they are treatable. People affected by these conditions are living their best lives with supportive medications to suppress and modulate the immune system, in addition to healthy lifestyle habits.
Common autoimmune conditions people with T1D develop are:
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
- Rheumatoid arthritis (RA)
- Lupus
- Multiple sclerosis (MS)
- Scleroderma
- Psoriasis
- Psoriatic arthritis
- Thyroid disease (Hashimoto’s thyroiditis)
- Celiac disease
- Adrenal insufficiency
Some individuals may never develop more than one condition. Others may develop autoimmune conditions in clusters, which is also known as multiple autoimmune syndrome.
The T1D Exchange Online Community and autoimmunity
To discover what autoimmune diseases the T1D Exchange Online Community lives with, a recent “Question of the Day” asked:
“In addition to T1D, how many other autoimmune diseases do you live with?”
Here is a breakdown of the responses:
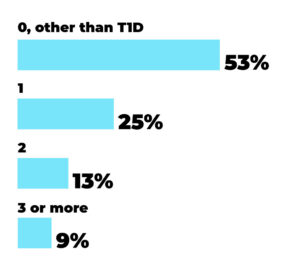
The most common “Question of the Day” responses were:
- Hashimoto’s thyroiditis
- Psoriasis
- Rheumatoid arthritis
- Fibromyalgia
- Celiac disease
Popular comments from the community include:
- “I’ll bet a lot of people don’t know they have autoimmune diseases, based on the percentage of “no” answers. Also, once we are diagnosed with one, it’s not always (not usually?) explained that it is an autoimmune disease.”
- “Autoimmune conditions run in my mother’s family.
I have hypothyroidism, as does everyone else in the family. I also have epilepsy due to GAD antibodies that most likely caused my diabetes. Microscopic colitis, and Raynaud syndrome.” - “I have so many autoimmune diseases, I don’t even know if I know them all. Hypothyroid, pemphigoid, asthma, celiac disease. The list goes on. I’m not sure anymore which ones are autoimmune diseases.”
- “I seem to be diagnosed with a new autoimmune disease regularly. Most significant being CIDP chronic inflammatory demyelinating polyneuropathy. Another is burning mouth syndrome which has a surprising effect on my quality of life. Several skin conditions which effect the use of my insulin pump and CGM.”
Symptom awareness
utoimmune conditions can affect single systems in the body or multiple systems all at once. As you can imagine, this often leads to confusion, extending the timeline for care and treatment.
Moreover, receiving a proper diagnosis for autoimmune disease can be challenging. According to research, the average time it takes to receive an autoimmune condition diagnosis is about 4.5 years — in addition to appointments with 4 different physicians.
With autoimmune disease, it is more important than ever to advocate for your care. You can do this by tracking your symptoms, vocalizing concerns to your care team, seeking other opinions, and becoming more educated about autoimmune disease in general. Let’s look at symptoms that can occur in different body systems.
Common autoimmune symptoms include (but are not limited to) the following:
Musculoskeletal: Warm, painful, and swollen joints, decreased mobility
Gastrointestinal: Indigestion, diarrhea/constipation, mucous, bleeding, bloating
Dermatologic: Skin sensitivities/changes, rashes, lesions, hair loss
Neurologic: Blurry vision, changes in sensation, memory issues, seizures
Endocrine Glands: Hormonal imbalances, fatigue, weight fluctuations, mood changes
Vascular: Skin ulcerations, vascular inflammation, fatigue, pain, fever
Vision: Sensitivity to light, dry eye, redness, blurry vision
If you have one or more of these symptoms, especially if they persist or worsen over time, consider talking to your care team. You deserve to feel your absolute best, so don’t let these symptoms become your “new normal.”
Testing for Autoimmune Conditions
There is not one specific test to diagnose all autoimmune conditions, but some are easier to diagnose than others.
Once you see your healthcare provider for a physical exam, they may consider additional testing. During this process, it is important to communicate with your care team that you already live with T1D, which is an autoimmune disease.
Various tests can be performed to help determine if you have developed a new autoimmune condition. The goal of testing is to identify, diagnose, and treat your symptoms.
They may order one or more of the following screening tests:
- Antinuclear antibody test
- Autoantibody tests
- Complete blood count
- Comprehensive metabolic panel
- C-reactive protein
- Erythrocyte sedimentation rate
- Urinalysis, and others
Keep in mind, this process will not begin until you share your experience with your care team. Autoimmune disease can affect healthy cells, tissues, and organs in any part of the body. If you are concerned about symptoms you’ve been having, advocate for yourself. Early diagnosis and treatment can help protect your organs and tissues while improving your quality of life.
Resources and Support
At T1D Exchange, we are committed to improving healthcare and outcomes for people living with T1D. We understand having trusted sources of information and support for healthy coping is important for your health. Consider digging into the following resources to learn more
- The Autoimmune Association offers support groups, patient apps, and additional autoimmune resources
- The T1D Exchange offers scientific information and research on T1D and autoimmunity
- The Global Autoimmunity Institute offers information about autoimmune-focused organizations and medical institutions, as well as books, podcasts, and apps