
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
Insulin is a key player in regulating blood glucose (BG), but it doesn’t act alone. Another hormone called glucagon plays a part as well. Glucagon has the opposite effect of insulin: It raises your BG. For this reason, many insulin users, including people living with type 1 diabetes (T1D), keep glucagon on hand in case of severe hypoglycemia, or low BG.
Besides treating severely low glucose, glucagon might also make it easier to keep your BG within target range in the first place. Scientists are exploring whether glucagon can improve BG management during exercise and after meals when it’s used with an automated insulin delivery (AID) system. Read on to learn about the different ways glucagon may be able to help people living with T1D.
Responding to severe hypoglycemia
Managing BG with insulin therapy is challenging at best. Hypoglycemia (BG <70 mg/dl) can happen unexpectedly. Often, consuming fast-acting carbohydrates, such as juice or glucose tablets, can treat hypoglycemia. But sometimes, you may be unaware that your BG is low, or your BG might not respond to the carbs you consume. In these cases, hypoglycemia can become severe.
Severe hypoglycemia is both scary and dangerous. It can cause dizziness, confusion, loss of consciousness, and seizures. In rare cases, it can be life-threatening. If you have severe hypoglycemia (BG <54 mg/dl), you may not be able to safely eat or drink, and you may need the help of others. In these situations, glucagon may be necessary to quickly raise your BG to a safe level.
Today, emergency glucagon comes in several formulations. Nasal glucagon (Baqsimi®) is a fine powder given through the nose, much like a nasal spray. Ready-to-use glucagon injectors (Gvoke®, Zegalogue®) are also available. Similar to other medications like epinephrine, you can also get syringes that are pre-filled with glucagon.
These options are easier to use than older glucagon kits, which involve several steps. Users had to mix powered glucagon with liquid in a vial, then draw the solution into a syringe for injection.
Newer formulations don’t require drawing up or mixing, and some don’t involve a syringe at all. They are also more portable; some dispensers are small enough to carry in a purse or waist pack. Glucagon can even be self-administered if necessary.
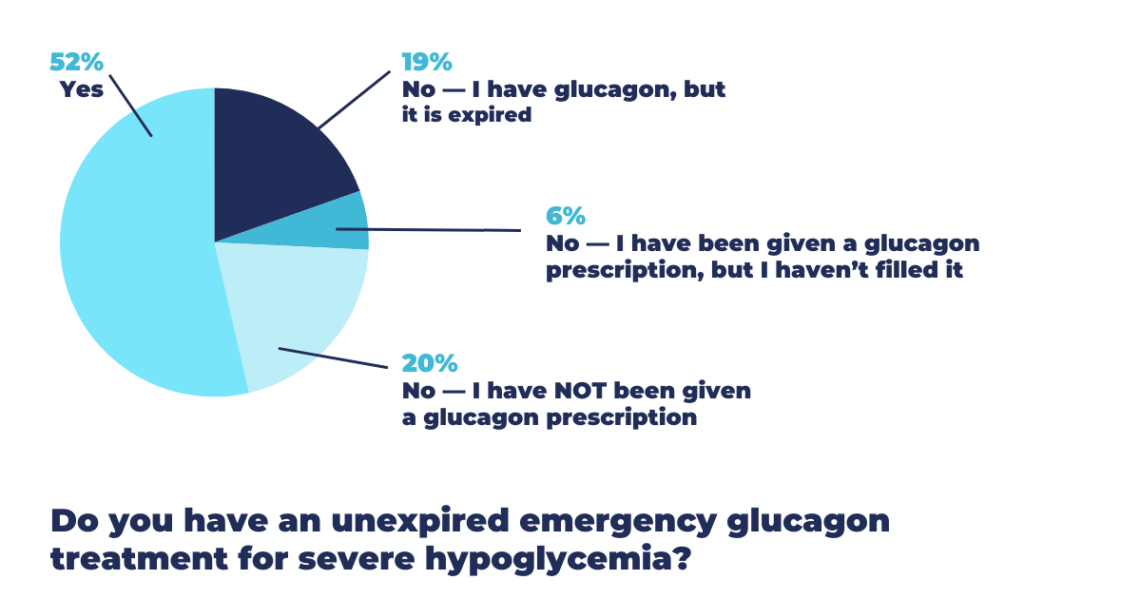
T1D Exchange recently asked our Online Community about emergency glucagon. Almost 250 people responded. Only about half (52%) have an unexpired emergency glucagon treatment for severe hypoglycemia. Other respondents never received a prescription (20%) or have an expired (19%) or unfilled prescription (6%) for glucagon.
There are many reasons why someone might not have current emergency glucagon available. They may not understand its importance, know how to use it, or be able to access it. This creates an opportunity to increase the adoption of this potentially life-saving medication.
Preventing low BG after exercise
Many people living with T1D notice that their BG drops during and after exercise. Some people try to prevent this by reducing their insulin dose or ingesting carbs, but these strategies have their drawbacks and don’t always work. That’s why scientists have proposed taking a small amount of glucagon (or a mini-dose) instead.
In research studies, mini-dose glucagon seemed to prevent hypoglycemia better than other strategies. However, we don’t know yet whether mini-dose glucagon works as well in real-world settings.
Speeding up insulin at mealtime
Besides raising BG levels, glucagon can increase blood flow, which speeds up several processes in the body. Researchers are testing whether it can help insulin work faster. This could be a big plus in keeping BG levels steady around mealtimes.
BG typically rises right after you eat, much faster than insulin can respond. This is why many people who live with T1D time their insulin dose before meals.
In response, researchers tried mixing insulin with a tiny amount of glucagon. In lab experiments, this mixture started working up to 10 minutes sooner than the fastest insulins on the market. A clinical trial to see how this insulin-glucagon formulation works in humans is now underway in Norway.
Dual-hormone delivery systems
Many people living with T1D use automated insulin delivery (AID) systems. These systems can make BG management easier and more effective, but they are not perfect. One problem is that they cannot react quickly enough when BG levels fall. While they adjust insulin delivery or suggest you ingest carbs, they can’t directly raise BG levels.
To address this, scientists are trying to upgrade AID systems with this capacity. One way to do this is by delivering glucagon. At least four different versions of dual-hormone delivery systems are currently in development.
- iLet Duo by Beta Bionics: An insulin-only version of this system is already on the market. Development of the dual-hormone version continues.
- Gemini by SFC Fluidics: The company received federal funding to launch clinical trials of its system in 2023.
- Inreda AP by Inreda Diabetic: This system showed promising results earlier this year. A larger clinical trial is now enrolling in the Netherlands.
- DiaCon Artificial Pancreas by The Copenhagen Diabetes Control group: A research group in Denmark has begun clinical testing of its experimental system.
By delivering insulin and glucagon as needed, these systems would better match how the pancreas works in people without diabetes. In turn, this could decrease some of the worry and burden associated with managing T1D. In systems like these — and the other applications described here — glucagon could help make everyday life easier and safer for those affected by T1D.







