Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
Move over A1C? Well, not so fast. While we rely more and more on data points from wearable continuous glucose monitors (CGMs) to assess and self-manage type 1 diabetes (T1D), A1C testing still has its place.
This being the case, perhaps you’ve noticed your diabetes care team increasingly focused on metrics like Time-in-Range (TIR) and Glucose Management Indicator (GMI) — and less on A1C.
Either way, the value of CGMs is indisputable. Users can view real-time and retrospective data to gain a clearer picture of their overall day-to-day.
Unlike a single A1C number, which reflects average glucose values over the past 90 days, with CGM data, you can adjust the viewing window — zoom in and out — identify patterns, and see percentages of time spent in, above, and below range.
Let’s take a look at the details.
_____________________________________________
What is “Time-in-Range” (TIR)?
Time-in Range is exactly what it sounds like: The amount of time you spend in your target glucose range. For most people, that’s typically 70% of the day in a 70-180 mg/dL range. But this may vary depending on the individual.
Beyond the safety mechanisms associated with CGMs, most people appreciate the accessibility of their CGM data and insights. Because of this, we can make timely and informed adjustments to minimize both hypo- and hyperglycemia.
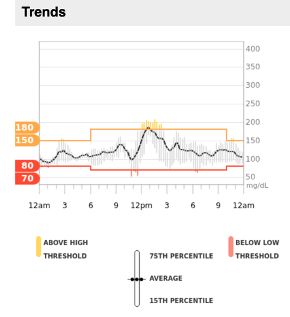
Take this Dexcom G7 report, for example. Even though my average glucose has been fine, I’ve been trending higher between noon and 3 PM lately. After seeing this, I’ve started paying more attention to my habits and pump settings during this time of the day.
How do I find my Time-in-Range report?
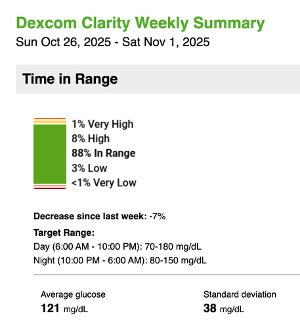
You can check your CGM data through your device-specific app — each manufacturer has its own. Dexcom users, like me, can also receive a weekly email with their Clarity summary.
Honestly, this is more helpful than anything. With data right under my nose, I can quickly get an overview of what’s been happening and dig deeper, if needed.
If you enable notifications, here’s the summary you can expect to receive:
What is an A1C?
Hemoglobin A1C, or A1C, measures your average glucose over the past few months.
Here’s how it works: Glucose sticks to red blood cells. The more glucose in your blood, the higher your A1C will be. Since red blood cells live for about 90 days, the test measures glucose over that period of time.
GMI vs A1C: What’s the difference?
GMI and A1C are two different metrics that measure glucose levels in the body. GMI is calculated from CGM data, giving a recent snapshot of glucose trends. A1C, on the other hand, is a blood test that provides an average glucose over a longer period.
If you’re finding discrepancies between GMI and A1C, that’s expected, given the difference in what they measure, explained Jennifer Okemah, MS, RDN, CDCES. “GMI data is more heavily weighted over the past two weeks, so it more accurately represents what’s happening right now.”
“GMI is a snapshot of what we’re working with, given that someone continues with their current patterns,” she said. “The reality is, when someone comes in with an elevated A1C, I’d want to see the latest data (GMI) to understand what’s been happening most recently.”
“That’s why I encourage people to ‘let go of’ a previous A1C,” it reflects what happened months ago.
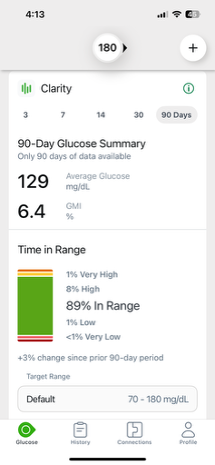
Where can I find my GMI?
Again, pull up your device-specific app. You should find what you’re looking for in the “reports” section and immediately generate a handful of glucose statistics. For Dexcom G7, you can adjust the timeframe you’re interested in, and it will calculate your average glucose and GMI.
Looking Ahead
A1C testing has been the standard for over 30 years, with research from the Diabetes Control and Complications Trial (DCCT) establishing a link between A1C values and microvascular changes in individuals with T1D. A newer consensus statement now provides recommendations for utilizing CGM data to complement A1C in clinical studies.
Moreover, researchers recently revisited the DCCT with a modern approach, finding that 14-day CGM data predicted microvascular changes similarly to A1C testing.
“A1C doesn’t tell the whole story, and while we’ve always known this, it was our only measurement tool. Now, many clinicians are questioning whether A1C is still necessary,” said Okemah, after attending the ADA 2025 Scientific Sessions. It’s not as telling or dynamic as CGM data.
For now, it’s recommended to evaluate GMI and A1C, but it’s worth noting recent research suggests AI could potentially be used to reduce the discrepancy between GMI and A1C results.