
Sign up for a new account.
And get access to
The latest T1D content
Research that matters
Our daily questions
Sign up by entering your info below.
Reset Your Password
Don't worry.
We will email you instructions to reset your
password.
Maybe you’re pregnant, or actively planning a pregnancy, or you want to know what to expect when that time comes. I think from child-bearing age, people with type 1 diabetes (T1D) are often filled with fear around the idea of pregnancy.
While it’s important to know the potential risks and complications, I won’t get into those here. Instead, I’ll focus on goals and a few things to expect throughout a T1D pregnancy — because an informed, goal-oriented mindset is more empowering than a fear-based mindset. I’ll also share some words of wisdom along the way from women who have gone through or are currently going through a T1D pregnancy.
When you look at the words within blogs and Instagram posts related to pregnancy with T1D, it doesn’t take long to get a sense of what it feels like for many people. These words are incredibly common when talking about pregnancy with T1D:
Reading through all of these personal accounts, the takeaway message is that yes, a healthy T1D pregnancy is challenging, but possible.
T1D Pregnancy: A1c and Blood Glucose Goals
Blood glucose management is at the core of a healthy T1D pregnancy. Your A1c and blood glucose goals will likely be lower during pregnancy than they’ve been during any other time in your life with T1D. While this may sound like a real challenge, it is possible to achieve with support from your team and other pregnancy resources. Once you know your goals, you can adapt your diabetes management strategies to meet them. (Remember, other people have done this! If they can do it — you can do it.)
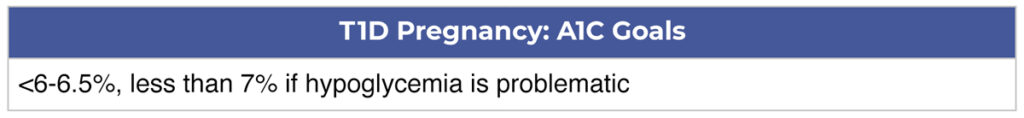
A1c
Recommended A1c goals before conception and during pregnancy are less than 6-6.5%, or less than 7% if frequent hypoglycemia is a problem.
“I always believed I could do anything living with T1D since the age of 12. However, pregnancy was the one challenge I felt the most intimidated by. Learning new strategies with insulin like pre-bolusing, pairing protein with carbs, movement and trusting that my body could do this are just some of the ways that I’ve been able to accomplish the A1c I’ve needed to support a healthy pregnancy.” – Brittany, currently pregnant with T1D (Instagram)
Blood Glucose
While the gold standard blood glucose range for people with diabetes is 70-180 mg/dL, blood glucose goals are lower to support a healthy pregnancy.
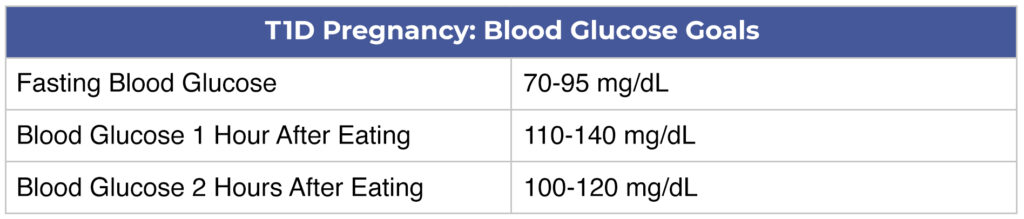
“Going into my pregnancy I was worried about whether I would hit my blood sugar targets which were lower than my usual goals. I was acutely aware of the potential complications of hyperglycemia during pregnancy and the increased challenges to blood sugar management. Now that I’m on the other side, I know that, with attention and effort, not to mention the powerful motivation of wanting to do my best for my baby, it is possible. Fortunately, I found that there were concrete steps I could take to help me reach my goals. First, even before I became pregnant, I began working towards my pregnancy blood sugar targets so that when I became pregnant I wasn’t trying to adapt my routine with the added stress of pregnancy.” – Jennifer Hildner (Instagram)
CGM and Target Range
With an emphasis on maintaining blood glucose goals during pregnancy, continuous glucose monitoring devices (CGM) may be helpful. CGMs provide real-time glucose measurements to help inform insulin, carbohydrate, and physical activity decisions.
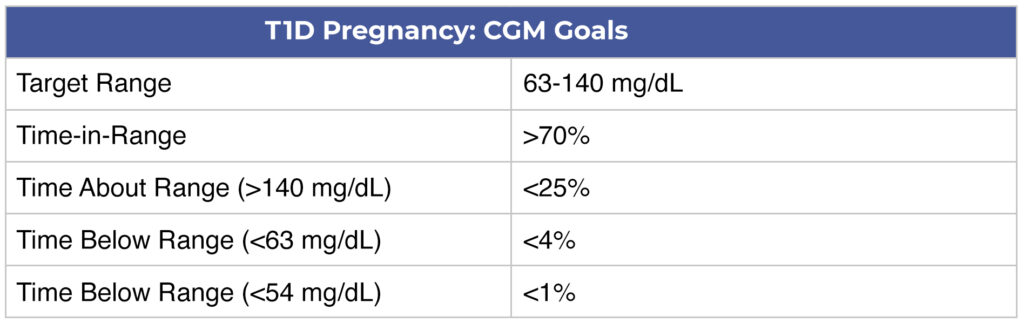
“Second, utilizing technology, specifically my continuous glucose monitor (CGM) and insulin pump, was incredibly helpful. I tightened my blood sugar targets on my CGM and decreased the ‘snooze’ time of my alerts to focus my attention when my blood sugars were out of range. I also leaned on my husband for support by, for example, sharing my CGM readings via the app to his phone and setting alerts on his phone so that he could wake me up in the middle of the night if I didn’t hear my phone’s alerts. Third, prioritizing regular exercise, even a short walk, was beneficial.” – Jennifer Hildner (Instagram)
T1D Pregnancy: Changing Insulin Needs
Now that you know your blood glucose goals for pregnancy, be aware that your insulin needs will change drastically throughout pregnancy — and you can blame hormones for that! It is natural and healthy for your insulin needs to be significantly higher than your non-pregnant doses by the time your baby is born. But you will be working hard to fine-tune for changes in insulin sensitivity, insulin resistance, and increasing insulin needs. Knowing when to expect these changes can help.
First Trimester: Insulin Sensitivity
Insulin sensitivity increases during early pregnancy (the first 13 weeks). This can lead to lower than usual blood glucose levels and decreased insulin needs. It’s important to be on the lookout for problematic hypoglycemia during this time and adjust your insulin doses accordingly.
Second Trimester: Insulin Resistance
Insulin resistance starts to show itself around 16 weeks into the pregnancy. You can expect your total insulin needs to increase by about 5% every week. Monitor your blood glucose levels closely so you can notice when insulin resistance starts to kick in and ramps up. You’ll notice changes in both your basal and bolus insulin doses.
Third Trimester: Insulin Resistance
Insulin resistance continues to increase well into the third trimester, up until around 36 weeks. During this time, you can continue to expect a 5% increase per week in your insulin needs. This means that your usual daily insulin needs could double by the end of your pregnancy.
Take-home Message
Every pregnancy experience is different, and having a T1D pregnancy can add extra challenges. Anticipating changing insulin needs and working towards specific blood glucose goals can help you to have a healthy pregnancy. Despite the insulin resistance, anxiety, and stress, the challenge of bringing a healthy baby into the world is worth it. Don’t be afraid to let others support you and remember to give yourself a little grace for every moment when things don’t go perfectly.
And on that note, I’ll leave you with a few final words of inspiration:
“If I could go back and speak to my former pregnant self, I would say, “Be kind to yourself and, also, you’ve got this.” – Jennifer Hildner (Instagram)
“It is intense management but I believe anyone can do it if they want to!” – Brittany, currently pregnant with T1D (Instagram)







